In many mid- to large-sized companies, the promise of new HR software is undeniable: greater
Learn more
If you’ve ever felt abandoned in the middle of a software rollout or watched your HR system launch
Learn more
In today’s digital age, HR teams are under growing pressure to modernize. New HR platforms,
Learn more
When organizations launch a request for proposal (RFP) to select a human capital management (HCM)
Learn more
As we approach 2026, the role of Human Resources is transforming, not gradually, but fundamentally.
Learn more
Human Capital Management (HCM) has evolved far beyond a “nice-to-have” software tool. In today’s
Learn more
We recently hosted a webinar titled “Avoiding Common HCM Software Mistakes”, and what stood out
Learn more
In HR circles, you'll hear a lot about HRIS, HRMS, talent platforms, and HCM, sometimes
Learn more
As ACA compliance continues to evolve, HR teams are facing a more complex and higher-stakes
Learn more
For HR professionals in the U.S., managing ACA compliance can feel like juggling flaming torches
Learn more
Now that you’ve scoped the countdown, it’s time for the next step: taking action and planning for
Learn more
As the end of the year approaches, HR and payroll teams face one of their most intensive windows:
Learn more
Retirement rules got you scratching your head? Don’t worry, Greg Duval, COO of FUSE, has your back.
Learn more
HR professionals are often the silent guardians of employee financial well-being. Payroll,
Learn more
If you work in HR or payroll, you’ve likely heard the buzz around the One Big Beautiful Bill Act
Learn more
Every new law brings questions. For HR professionals and payroll teams, that’s especially true
Learn more
Changes big and small tend to land on HR’s doorstep and the One Big Beautiful Bill Act (OBBBA) is
Learn more
You nailed communication (Part 3), you energized benefits (Part 2), you tamed chaos (Part 1), but
Learn more
You know that moment when you finally send out your open enrollment email … and hear absolutely
Learn more
Open enrollment is often seen as HR’s annual fire drill. But here’s a thought: what if instead of
Learn more
If you’ve ever lived through open enrollment season, you know it’s not all pumpkin spice and cozy
Learn more
In manufacturing, collective bargaining agreements (CBAs) define the rules of engagement between
Learn more
As nonprofits grow, so can the challenges behind the scenes. More employees, more programs, more
Learn more
Today, manufacturers face complex labor dynamics, including shifting schedules, union rules, and
Learn more
Payroll is one of the more important and more stressful tasks nonprofit leaders face. Between tight
Learn more
The Fair Labor Standards Act (FLSA) sets the rules for minimum wage, overtime pay, and employee
Learn more
Are you wondering how long it takes to implement HR and payroll software? The answer depends on
Learn more
Implementing an HCM system can feel overwhelming. It doesn’t have to be with the right strategy and
Learn more
The best place to start when choosing HR software is with your goals. Before you compare features
Learn more
Change is a constant in today’s workplace. Whether that may be rolling out new technology, shifting
Learn more
You know your current HR or payroll system isn’t cutting it. Maybe it’s clunky. Maybe it’s manual.
Learn more
The rise of AI is transforming the workplace at a pace few anticipated. From automating routine
Learn more
Companies often need to make tough decisions about their workforce in the face of changing market
Learn more
Recruitment is at the heart of every organization’s success, yet traditional hiring processes often
Learn more
In payroll management, accruals keep track of employee benefits like paid time off (PTO) and sick
Learn more
Have you ever struggled to manage multiple logins across various HR and payroll systems? In today’s
Learn more
Companies must adapt to new challenges and evolving market conditions to stay competitive in
Learn more
Managing Time, Attendance, and Scheduling in 24/7 Healthcare Environments Hospitals don’t close for
Learn more
HR leaders in healthcare navigate some of the most complex challenges in the workforce. Every shift
Learn more
In healthcare, time isn’t flexible—and neither are the demands on your workforce. While nurses
Learn more
HR used to rely on instincts and experience to make workforce decisions. Now, data is changing the
Learn more
Resumes are screened in seconds, engagement issues flagged before they escalate, and workforce
Learn more
Remote work has transformed from a temporary solution into a long-term expectation. However, as
Learn more
Finding the right talent has become both a science and an art in today's society. Traditional
Learn more
Hiring managers and recruiters share the same goal: securing top-tier candidates quickly and
Learn more
Job descriptions shape the hiring experience, influencing who applies and how well candidates match
Learn more
Companies invest millions in training programs yearly, yet studies show that 70% of employees
Learn more
Administrative tasks are the silent engine of HR operations, but when managed manually, they can
Learn more
It’s no secret that effective onboarding is the critical first step in employee retention and
Learn more
Traditional performance reviews often fail to meet expectations. They’re infrequent,
Learn more
Performance reviews are a tool for nurturing employee growth, aligning them with company goals, and
Learn more
The interview process is a critical part of hiring that shapes candidates' perceptions of your
Learn more
Companies constantly seek innovative ways to attract and retain top talent in today's competitive
Learn more
Employee productivity is the motor that drives any successful business, influencing everything from
Learn more
The payroll landscape is evolving, driven by the demand for flexible, real-time, and
Learn more
As businesses seek new ways to support their employees’ financial well-being, concepts like earned
Learn more
In today's competitive job market, attracting and retaining top talent is more challenging than
Learn more
As the year draws to a close, businesses everywhere are gearing up for the flurry of year-end
Learn more
The COVID-19 pandemic triggered a massive shift to remote work almost overnight, transforming the
Learn more
Employee retention is a critical aspect of maintaining a successful business. While various factors
Learn more
Today's work culture is more demanding and fast-paced than ever before, often straining employees'
Learn more
In today's competitive job market, having a strong employer brand is crucial for attracting and
Learn more
In the ever-evolving world of work, company culture has become a critical factor in business
Learn more
In the fast-paced business world, having an efficient and reliable payroll system is not just a
Learn more
Succession planning software is designed to help organizations identify and develop internal
Learn more
Let me start with a cautionary tale that's been played out far too often. A new business venture
Learn more
Discover the benefits of implementing mentorship programs for employees and how they can contribute
Learn more
Explore the critical role HR plays in fostering employee learning and development within
Learn more
Discover the numerous advantages of implementing a Learning Management System (LMS) in your
Learn more
Discover the key differences in payroll and HR requirements between companies that predominantly
Learn more
Discover the significance of managing time off requests to ensure a productive work environment and
Learn more
Understanding what an Enterprise Resource Planning (ERP) system and an all-in-one payroll and HR
Learn more
Unlock the potential of HR analytics to revolutionize your hiring process HR analytics has the
Learn more
Understanding the Limitations of Big-Name Payroll and HR Companies Many businesses are finding that
Learn more
As you enter the fourth quarter of the year, there’s a lot that HR needs to get done. It’s not just
Learn more
Discover how implementing an employee self-service (ESS) portal can significantly enhance employee
Learn more
Discover the essential strategies top HR recruiters use to attract and hire the best talent in any
Learn more
Artificial Intelligence (AI) is making its mark across various aspects of our professional lives,
Learn more
At the onset of the global pandemic, a significant transformation took place in the corporate
Learn more
In the world of Human Resources, we often hear new buzzwords. Everyone's been talking about
Learn more
Seasonal hiring is a problematic situation for businesses to navigate. Done right, it can help your
Learn more
An often overlooked area of recruiting is how to find hourly employees. Hourly workers are becoming
Learn more
In today's competitive employee marketplace, retaining young talent like recent college graduates
Learn more
In today's rapidly evolving world, diversity isn't just about filling a quota. It's a dynamic
Learn more
Recruiting continues to be a fundamental pillar of human resources management. An organization is
Learn more
In the world of human resources, there are different types of software systems that help manage
Learn more
Employee retention is a top priority for organizations in today’s competitive market. High turnover
Learn more
Employee retention is a critical factor for any organization's success. Losing valuable employees
Learn more
Employee retention is a critical factor in the success of any organization. High employee turnover
Learn more
In recent years, the concept of relational human resources (HR) has gained increased attention
Learn more
What is an HRIS Integration? A Human Resources Information System (HRIS) integration involves
Learn more
Understanding employee satisfaction is essential for today’s economy where we have people coming
Learn more
Training is one of the most effective ways to improve employee performance. It is also
Learn more
No matter the size of your organization, one metric you can't shake free of is worker productivity.
Learn more
Talent retention is a significant concern for organizations, so it's important to understand the
Learn more
Creating a diverse workforce is important for any business to thrive. As such, many companies
Learn more
While understanding what it costs to hire an employee has always been important, as we look at
Learn more
A key component of effective workforce management is staying on top of critical dates and
Learn more
Building a culture that incorporates diversity, equity, and inclusion (DEI) is critical to
Learn more
When the pandemic began, many organizations were forced to send employees home, whereas others had
Learn more
Employee onboarding is so much more than the old-fashioned notion of orientation. Unlike a single
Learn more
Helping employees reach their full potential and career goals is essential to support a positive
Learn more
Performance reviews—whether conducted annually, quarterly, or on some other schedule—are an
Learn more
Though you probably offer a combination of constructive feedback and coaching to employees, there
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
Creating a highly engaged workforce has been a longtime goal for many organizations, as engaged
Learn more
Affordable Care Act (ACA) tracking is a must for employers, but what are the key components that
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
The latest advances in modern technology mean you now have access to dynamic tools that support a
Learn more
Just about every talent management activity generates data. From the moment candidates apply to the
Learn more
A human resources business partner (HRBP) is a critical member of the HR team, helping the
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
The Affordable Care Act (ACA) became law in 2010, and it has since made healthcare more accessible
Learn more
An essential part of effective payroll management is periodically auditing your payroll policies
Learn more
A unified workforce management system ties together all of the core elements of a talent management
Learn more
Whether you have a few non-exempt employees earning overtime or many more, managing overtime costs
Learn more
When you have a mobile workforce, some or all of your employees perform their duties outside of a
Learn more
Even with a solid payroll process in place, payroll errors still occur. Miscommunication between HR
Learn more
Reliable HR metrics help you understand the success of people initiatives, as well as their
Learn more
Errors and delays in payroll can be frustrating for everyone—payroll staff, HR, and the impacted
Learn more
Having an accurate count of employee hours enables you to manage what is likely your organization’s
Learn more
Getting payroll right is essential for delivering an exceptional employee experience and staying in
Learn more
For busy HR and payroll professionals, every month of the year brings new deliverables, and there
Learn more
Effective payroll management requires making sure your employees receive correct payments, on time,
Learn more
Keeping track of your manufacturing labor force requires specific tools and resources to help you
Learn more
How and where you store HR data is more important than you might think. It impacts the efficiency
Learn more
In an area as broad as HR, it’s easy to get pulled in several different directions. When running a
Learn more
Performance reviews can take many forms, from informal weekly check-ins to quarterly or
Learn more
Preparing your workforce to meet the challenges of tomorrow requires a robust talent development
Learn more
When you have a highly engaged workforce, your organization is in a better position to achieve its
Learn more
As a human resources leader, you’re responsible for delivering programs that improve the employee
Learn more
Payroll duties require careful strategy, teamwork, and execution. You have to deal with numbers and
Learn more
Whether you’ve been in Human Resources for 25 years or you’re just starting out your career, the HR
Learn more
In the market for a new payroll provider? Ready to move to the cloud? You've got some research
Learn more
Your payroll manager is key to your organization’s smooth operations. After all, they are
Learn more
Your payroll provider is responsible for helping you deliver accurate employee pay, but if the
Learn more
From the moment an employee becomes part of your organization, they rely on support from your HR
Learn more
An integrated HR payroll system is a software solution that merges payroll and HR activities for
Learn more
When you manage several HR processes at once, you rely on automation technology to get more
Learn more
As an HR professional, you’re responsible for coordinating everything that comes along with human
Learn more
As countries around the world enforce stay-at-home orders, employees across industries and
Learn more
The most productive HR teams rely on effective business reporting, but with so many staff members
Learn more
On April 1st, we held a webinar to discuss the details of the Families First Coronavirus Response
Learn more
With the holidays behind us and the new year in full swing, many workplaces may be actively trying
Learn more
It’s possible to attach a metric to just about any HR activity. However, not all HR metrics deliver
Learn more
Losing your best employees is a bummer. It takes a lot of time and resources to find a replacement
Learn more
With the start of the new year, it’s time to start looking ahead to what the next 12 months have in
Learn more
This year has been an eventful one for workplaces all over the United States. Between legislative
Learn more
For time-strapped HR and payroll managers, every day at work is a juggling act. The mental load of
Learn more
It’s no secret that social media has become part of most peoples’ daily routines in the last few
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
With Thanksgiving coming up later this week, the holiday season is in full swing. In offices around
Learn more
Many modern employers are focused on improving employee engagement metrics, and for good reason:
Learn more
Elementary school teachers and parents of young children have long been known to use sticker charts
Learn more
As competition for the best talent heats up in most industries, it’s important for recruiters and
Learn more
When an employee chooses to leave your company for another opportunity, it’s understandable that
Learn more
When your best employees leave, they don’t just take their skills and training with them; they also
Learn more
Autumn doesn’t just bring change to the leaves outside; there’s plenty of change happening in
Learn more
The Occupational Safety and Health Administration (OSHA), which falls under the larger umbrella of
Learn more
For anyone who loves variety and thrives in a busy job, working in HR may be a great fit. The role
Learn more
Distraction is an epidemic in nearly every modern workplace. Between the rising popularity of open
Learn more
For some people, the end of August means back-to-school shopping and parent-teacher conferences.
Learn more
If you’ve been in HR for any amount of time, you’re aware of the myriad problems associated with
Learn more
As most HR managers can attest, employee turnover is pricey. In addition to the cost of lost
Learn more
Even in the best of times, keeping your recruiting operation running smoothly can be a challenge.
Learn more
As the dog days of summer wear on and the Supreme Court is done handing out verdicts about
Learn more
What’s the first thing you do before you buy a new piece of furniture? Visit a new restaurant? Book
Learn more
In 2018, a Bureau of Labor Statistics survey found workers were quitting their jobs at the highest
Learn more
Most employees do their best work (and enjoy the greatest sense of satisfaction) when they’re
Learn more
Q2 is coming to a close and summer is officially in full swing. As you reflect on the first half of
Learn more
Recruiting, hiring, and onboarding new talent is a time-consuming and expensive process. Sourcing
Learn more
Being responsible for hiring new employees means exercising due diligence to ensure the
Learn more
As an HR leader, you’re accustomed to helping others develop their skill sets and ascend through
Learn more
As summer draws closer and temperatures rise, May’s roundup proves things are heating up for the HR
Learn more
When it comes to making hiring decisions, most employers begin by evaluating hard skills —
Learn more
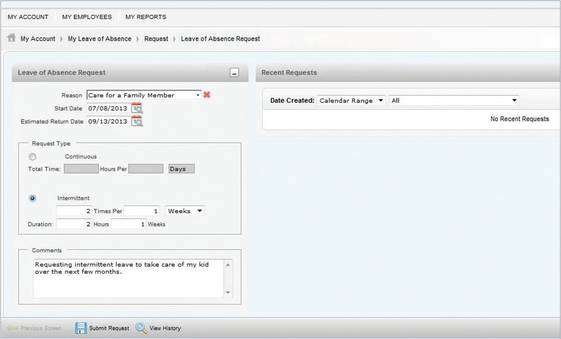
If administering the Family Medical Leave Act (FMLA) gives you an enormous headache, you’re not
Learn more
As an HR expert, your hiring decisions often hinge on a candidate’s performance in their job
Learn more
As we kick off the second quarter and resurface after a strenuous tax season, HR leaders are
Learn more
When legal conflicts arise between employees and employers — such as misconduct or a breach of
Learn more
Working in human resources is an enriching and rewarding career that allows you to make a
Learn more
As we round out the first quarter of the year and head into tax season, there are lots of changes
Learn more
When the COVID-19 pandemic began in early 2020, an unprecedented number of employees were sent to
Learn more
As a busy HR professional, finding time for career development can be challenging. While there are
Learn more
For most HR managers and company leaders, staying in compliance with employment law is a high
Learn more
The hiring process is crucial to the success of your workforce, especially when you’re filling an
Learn more
Most people who take pride in their work want to become more efficient, more effective, and
Learn more
Performance reviews can be a time for of delicate conversations, honest feedback, and thoughtful
Learn more
When you’re recruiting and hiring new employees, the right skills and experience are probably at
Learn more
With the first month of a new year coming to a close, employers are starting to get a feel for
Learn more
Happy New Year! As you’re putting together a list of resolutions, boosting your career as an HR
Learn more
You’ve made it through the holiday season: the company parties, the seasonal workers, the tricky
Learn more
Over the past few years, we’ve seen a big shift in the way people work due to changes in culture,
Learn more
Labor headwinds like demographic shifts and changing employee expectations have kept HR managers
Learn more
Read part 8: How an HCM system can improve productivity for HR, part eight: Retention While you
Learn more
The holiday season can be a tricky time for HR professionals and company leaders. Everyone on
Learn more
We’ve officially entered the holiday season, and we’re within striking distance of the new year.
Learn more
Read part 7: How an HCM system can improve productivity for HR, part seven: Compliance The grass
Learn more
If you’re in HR or payroll, you’re no stranger to compliance management, forms, and
Learn more
Read part 6: How an HCM system can improve productivity for HR, part six: Benefits Management
Learn more
With all the time-sensitive tasks HR managers are responsible for, it’s understandable that
Learn more
If October seems like the month for scary tricks, don’t forget there’s always something to sweeten
Learn more
HR managers, gather ‘round the fire for a truly scary ghost story. You’re trying to hire a few
Learn more
Traffic patterns, school schedules, family obligations, and doctor’s appointments can all break the
Learn more
Fuse Workforce Management has been identified as one of the best HR and Payroll Management Suites
Learn more
Making important decisions about employee benefits, like choosing health insurance packages, can be
Learn more
Happy National Payroll Week! All week long, we’re celebrating our beloved payroll professionals who
Learn more
Taking too long to hire the right person for a vacant position is almost guaranteed to cause
Learn more
A lot of trends between generations in the workforce have emerged in the past few years: Baby
Learn more
In this summer edition of the HR Roundup, a technology company inspires vacation for employee
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
What happens when state law and federal law disagree? Today in the U.S., over 20 states have laws
Learn more
Read part 4: How an HCM system can improve productivity for HR, part four: Payroll If you hear
Learn more
When people talk about making lateral career moves, the response from friends, family, and mentors
Learn more
The workforce is paradoxically both more dispersed and more connected than ever before. A manager
Learn more
Read part 3: How an HCM system can improve productivity for HR, part three: Training To many of us,
Learn more
In any role, the first few weeks are a virtual minefield of awkward experiences and newbie
Learn more
This April, we saw people take action for civil and labor rights, moving the tides in the HR
Learn more
When President Clinton first signed the Family and Medical Leave Act (FMLA) into law in 1993, the
Learn more
Read part 2: How an HCM system can improve HR productivity, part two: Onboarding So you’ve
Learn more
For new employees, the first few days and weeks on the job are crucial. So much of their future job
Learn more
Spring is coming, and there’s fresh news in the HR landscape. With March Madness over, there’s
Learn more
On the Fuse HR & Payroll blog, we’ve talked a lot about the many benefits of a human capital
Learn more
Read part 1: How HCM system can improve HR productivity: recruiting + hiring As an HR manager,
Learn more
In the past several decades, women have made huge strides in the workplace. All it takes is
Learn more
Next hurricane season, don’t expect your pizza delivery in the midst of an evacuation. Despite a
Learn more
You’ve probably noticed that the modern American workforce is changing. That may be partly due to
Learn more
The national conversation about sexual misconduct seems to have reached a flashpoint in the past
Learn more
We’re one month into 2018, and there’s plenty of HR news to report. For many workers across the
Learn more
At the end of 2017, the IRS began sending Letter 226J to Applicable Large Employers (ALEs) as a
Learn more
Fuse Workforce Management has been identified as one of the best software and services companies in
Learn more
In the 1970s, the Boston Symphony Orchestra (BSO) had a problem: an almost all-male orchestra. This
Learn more
As we closed out 2017, a wild year for regulatory changes and workplace legislation, we witnessed
Learn more
Don’t you love the beginning of another new year, with a blank calendar full of potential? By now
Learn more
To say that 2017 has been a turbulent year for many HR managers would be an understatement. Between
Learn more
Keeping up with the news on the Affordable Care Act is difficult, and maintaining ACA compliance
Learn more
As 2017 draws to a close, it’s time for leaders in every workplace to evaluate what’s worked well
Learn more
Lately, it seems you can’t look at the news without another sexual harassment scandal popping up.
Learn more
It’s that time of year again! Our HR and Payroll calendar has become a favorite among our blog
Learn more
This time of year, there’s an extremely contagious little bug that gets around in crowded places,
Learn more
While the future of healthcare in America has been uncertain for most of this year, the ACA 2017
Learn more
Since 1919, several allied countries who participated in World War I have observed November
Learn more
It’s long been a key feature of the postwar American dream: hardworking Americans look forward to
Learn more
Company leaders are (rightly) preoccupied with the buzzy concept of “corporate culture” these
Learn more
The Ban the Box movement is a grassroots effort aimed at changing hiring practices that make it
Learn more
From natural disasters to last-minute repeal efforts, September has been full of buzzworthy news.
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
In past articles, we’ve discussed the importance of having ongoing discussions about employee
Learn more
Happy National Payroll Week! Since its founding by the American Payroll Association in 1996, NPW
Learn more
Summer is coming to an end and school is back in session. In the spirit of learning, let’s take a
Learn more
While it seems a lot is up in the air with healthcare in America, employers are asking about the
Learn more
This month, all eyes have been locked on the Senate. Debates surrounding the Affordable Care Act
Learn more
In 1990, the Americans with Disabilities Act (ADA) was signed into law, prohibiting employers,
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
If you’re like many other HR professionals, recruiting, hiring, onboarding, training, and managing
Learn more
June marked the official beginning of summer—but that has not slowed down the happenings in the
Learn more
Get hired, learn your job and prove yourself, get promoted, prove yourself in that role, get
Learn more
If you’re a recent college graduate, things are looking up for you—much better than your Millennial
Learn more
Most employers have experienced how challenging it can be to keep employees engaged in the long
Learn more
What’s happening in the world of HR this month? Congress has been busy developing, refining, and
Learn more
Maybe it’s medical advancements that allow people to stay healthier and live longer. Maybe it’s the
Learn more
It's time for another HR Roundup of the latest HR news and trends. This month, we review the Trump
Learn more
When an employee chooses to leave your organization– either for a new job elsewhere, or because
Learn more
As we approach the summer break, more and more college students will start hunting for internship
Learn more
What’s been happening in the world of HR lately? Honestly, what hasn’t? If you’ve been keeping an
Learn more
As Women’s History Month draws to a close, it’s a good time to reflect on and celebrate the
Learn more
"Corporate culture" has become such a common HR buzzword that it may elicit some eyerolls from
Learn more
We all know that staying informed about what's going on in our industry is important. But in the
Learn more
A job application is the first contact many companies will have with potential future employees or,
Learn more
We can all agree that 2017 has turned out to be quite a year so far. A lot remains in question
Learn more
Sometimes setting goals for employees seems like an afterthought tacked onto the performance review
Learn more
In the past several years, more companies have started to employ a blended workforce, whether they
Learn more
While many of us were focused on year-end processes and keeping employees in check at the company
Learn more
Wellness programs have steadily grown in popularity in the last few years. According to a 2015
Learn more
At the beginning of this year, we published an article predicting workplace trends to watch for in
Learn more
There’s nothing dull about Human Resources these days. This fall has boasted a lot of change and
Learn more
Whether or not you believe in making new year’s resolutions, the end of the year can be a
Learn more
Finally, a compliance calendar for HR and Payroll! If you've ever wondered how to stay on top of
Learn more
November is here and everything year-end seems to be right around the corner. But before we dive
Learn more
While the prospect of creating or updating your paid time off policy may seem like a simple matter
Learn more
Before we get too lost in our PSLs and flannel shirts, let's talk about September. What a month in
Learn more
Monitoring employee engagement should be part of any productive organization. Not only do engaged
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
What’s new in HR news this month? The IRS and the DOL gifted us with new forms and posters for 2017
Learn more
Though it seems we’ve only just wrapped up ACA reporting in 2016, we’re already looking ahead to
Learn more
Bad news: sometimes, your most productive, positive, engaged employees will leave your company. It
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
Not long before summer’s start, the DOL announced the final rule for overtime and white-collar
Learn more
We may have barely made it through the 2016 deadline for ACA reporting but it’s time to start
Learn more
If you’re planning to expand your workforce, first of all: congratulations on the growth! But
Learn more
The reporting deadline for Form 1094-C and 1095-C electronic filing is Thursday, June 30, 2016. Is
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
As of the beginning of 2016, your company is responsible for proving compliance with the Affordable
Learn more
While some companies have taken these inherent flaws in the process as a sign that they need to
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
Once again, the time has come for another roundup of what's been happening in the world of Human
Learn more
HR managers routinely identify employee reviews as their least favorite part of the job. To most
Learn more
The Department of Labor’s proposed FLSA changes could change exemptions for as many as 5 million
Learn more
Here’s what you need to know about Human Resources lately. This article recaps recent HR news
Learn more
Raise your hand if you enjoy managing the annual employee review process. (Cue crickets). Nobody
Learn more
Finding the right talent for your company is a challenge even in the best of times. But with the
Learn more
For an HR manager, the onboarding process can potentially be a clipped, formal set of necessary
Learn more
There is a lot of information out there and it’s easy to get lost in the mix of it all. As a
Learn more
The process of finding the right employees for your organization is never a particularly easy one.
Learn more
If you’re trying to follow payroll best practices, you know manual payroll is a thing of the long
Learn more
The process of training new employees has so many moving parts that any company can easily let a
Learn more
An employee’s first few days are such a crucial and potentially awkward time for them. We’ve all
Learn more
The buzzword in benefits and compensation training these days is Total Rewards. In the competition
Learn more
Looking for the 2017 HR & Payroll Compliance Calendar? It's right here! We’re several weeks into
Learn more
Last week, the IRS opened its doors to begin receiving tax forms for the 2015 calendar year.
Learn more
We don't like to talk about ourselves much—we're here to serve you by streamlining your HR and
Learn more
The US Treasury and IRS recently announced extensions for Affordable Care Act reporting. Previous
Learn more
Much ink has already been spilled about what we’re supposed to anticipate in HR departments for the
Learn more
With 2016 just around the corner, you may be thinking of some personal and professional New Year’s
Learn more
Editor's Note: Since the publishing of this article, the IRS and U.S. Treasury extended reporting
Learn more
Editor's Note: Since the publishing of this article, the IRS and U.S. Treasury extended reporting
Learn more
A lot goes into ACA compliance, but many employers fear the financial penalties most. Are you aware
Learn more
Editor's Note: Since the publishing of this article, the IRS and U.S. Treasury extended reporting
Learn more
Shopping around for the right time and attendance software is no easy task. There are a lot of
Learn more
Consequences for ACA noncompliance have employers and human resources staff on their toes about
Learn more
Imagine showing up to a party where you know absolutely no one. Although you’ve been invited to the
Learn more
Pay day. A day to count down to and celebrate, right? The anticipation, the joy, the money! While
Learn more
Update: As of July 1, 2024 changes have been implemented to the Fair Labor Standards Act. For most
Learn more
Affordable Care Act (ACA) compliance and reporting—don’t do it right and your business will face
Learn more
With healthcare costs on the rise and large companies like Google offering monstrous employee perks
Learn more
It’s awkward. It’s uncomfortable. But at some point or another, you have to do it. While firing an
Learn more
Ah, the unpaid summer internship. For many college students, it’s viewed as a rite of passage, a
Learn more
The Department of Labor released its much-awaited proposals to the overtime rules in the Fair Labor
Learn more
The Fair Labor Standards Act of 1938 was a major win for workers in the United States. It
Learn more
Is your company’s push for employee engagement burning out your best people? Burnout happens when
Learn more
Annual performance reviews can be a source of dread for many supervisors. What could possibly be
Learn more
Hiring new college graduates is a great strategy for lots of reasons. They’re eager to get work
Learn more
Effective July 1, 2015, the Healthy Workplaces, Healthy Families Act of 2014 will impose new paid
Learn more
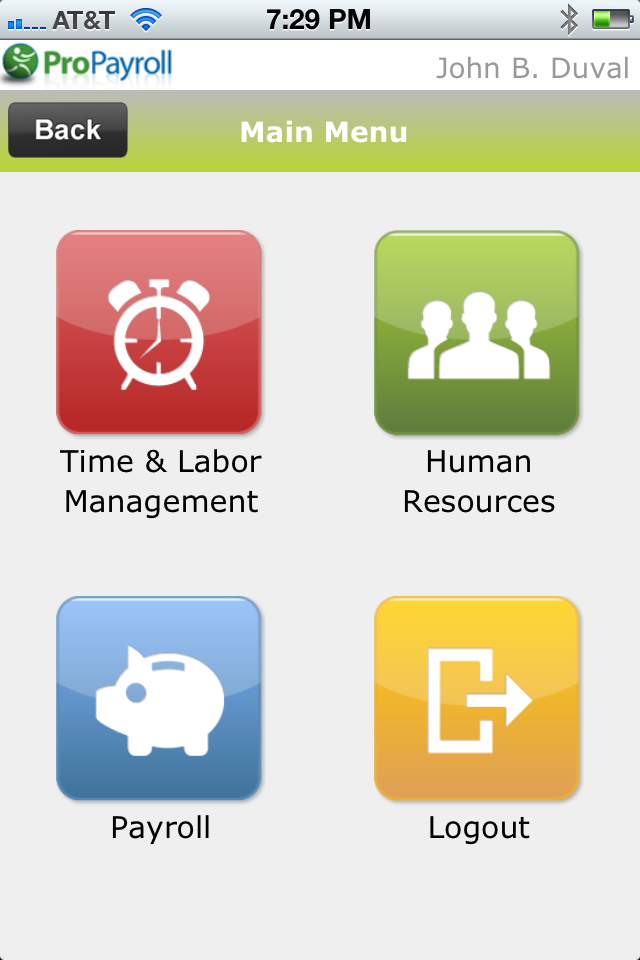
ProPayroll today announced the latest release of the Fuse Workforce Management suite - including
Learn more
ProPayroll Further Positioned to Capitalize on SMB Market with Workforce Management Platform
Learn more
appPicker.com has selected TotalHRWorks, ProPayroll’s mobile app, as a top app for Employee
Learn more
ACA Mandates Delayed for Employers with 50-99 Employees until 2016, and Requirements are Lightened
Learn more
Proactively manage ACA compliance across your entire workforce.
Learn more
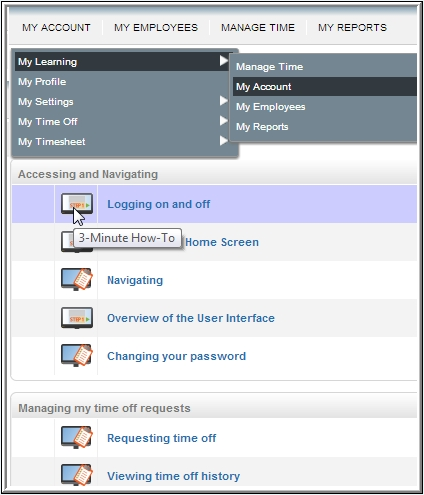
ProPayroll is excited to announce that we have released KnowledgePass to all clients and their
Learn more
As of October 1st, 2013, due to the government shutdown, The Department of Homeland Security will
Learn more
Please take note of the following changes to E-Verify guidelines in both Georgia and North
Learn more
ProPayroll Inc. today announced a series of enhancements to its fast-selling cloud workforce
Learn more
The term “Fiscal Cliff” was coined to refer to the convergence of several major events at the close
Learn more
E-Verify is now fully integrated into ProPayroll’s Workforce Management platform. E-Verify is a
Learn more
The Federal Reserve will be closed on Monday, October 8th in observation of Columbus Day. Follow
Learn more
The laws in the following states expressly permit, or can be interpreted as permitting, employers
Learn more
On August 13, 2012, the U.S. Citizenship and Immigration Services (USCIS) released a bulletin
Learn more
The ProPayroll Employee Handbook Wizard is now available within our HR Support Center. The wizard
Learn more
The ProPayroll paycard includes a great Rewards Program for your employees. Sign up for exciting
Learn more
Speed, going green, reducing paper costs, freeing up physical office space and avoiding shipping
Learn more
Historically, outsourcing payroll has been a necessary evil for many companies focused on their
Learn more
Businesses switch to online payroll companies for improved efficiencies, lower costs and better
Learn more
The Hiring Incentives to Restore Employment (HIRE) Act, also known as the “jobs bill”, that was
Learn more
 Human Resources, Latest News,
Human Resources, Latest News,





















































































































































































.png)





.jpg)

.jpg)